Building strong communities through blood donation
January is about new beginnings and fresh starts. It’s also National Blood Donor Month – a time to consider the important role blood donation plays in the health of our community.
Blood donation is critical for people involved in traumatic accidents, during medical operations and procedures, and also for people with cancer, anemia, and autoimmune disorders, among others.
The Red Cross reports that every two seconds, someone in our country needs blood or blood products.
Hospitals and health systems, like PacMed, Swedish and Providence, rely on local blood banks to maintain blood product supplies. However, COVID-19 has impacted donation volumes. Lifesaving blood donations remain essential for patients in need.
Help keep your community strong by donating blood locally. Find a donation center near you at https://www.redcrossblood.org/.
FAQs regarding blood donation and COVID-19:
Q: Is it safe to donate blood if you’ve had COVID-19?
A: Yes. If you’ve had COVID-19, you must be without symptoms for 14 days prior to blood donation. If you are asymptomatic, you must wait 14 days from the date of your positive test result.
Q: Will donating blood reduce COVID-19 fighting-antibodies?
A: No. If you’ve had the COVID-19 vaccine, your antibody levels won’t go down after you give blood, as your body will quickly replenish the antibodies.
Q: Will donating blood increase my exposure to COVID-19?
A: No. Donation centers take all necessary precautions to protect their donors and their staff members.
Q: Does my COVID-19 vaccination status impact my ability to donate blood?
A: Check with your local blood donation office to verify their COVID-19 vaccination requirements.
Mental & emotional health awareness and support for a better future
Warm 106.9: Mental and emotional health issues have either become more of a problem, or maybe we are beginning to be more open. Being open and seeking support is an important step. Serena touches on some aspects of the challenges of this season on our mental health, both the shorter and darker days as well as all the holidays and feelings of obligation.
If restoring function is a puzzle, this physician sees all the pieces
Care plans and treatments to help patients get back to the activities they love
In her third year of medical school, Tam Quach, DO, helped treat a severely debilitated patient with so many internal and external injuries, she couldn’t walk.
“By the time I left a month later, she was taking her first steps! It was very rewarding to see her progress,” Dr. Tam says.
Witnessing that transformation inspired Dr. Tam to specialize in Physiatry, also known as Physical Medicine and Rehabilitation, and now she’s bringing that practice to Pacific Medical Centers (PacMed) in Seattle.
“Physiatry focuses on restoring function,” she explains. “We treat anything that affects function, including brain injury, strokes, amputations, musculoskeletal pain and peripheral joint pain. We develop care plans to help patients get back to daily life.”
Continuum of care
Physiatrists are highly trained physicians who look at the whole body. Dr. Tam’s care plans include close collaboration with other specialists like physical therapists, surgeons and prosthetists, and can incorporate virtual visits for added convenience.
“We use a combination of therapy, medication and injections to get the patient’s quality of life back. We can’t always take away all pain, but our goal is to restore as much function as possible, and get you back to the things you enjoy,” she says.
The most common injury Dr. Tam treats is back pain, and she’s also very interested in amputee care.
“It’s important for patients to realize that their amputation doesn’t have to stop them from having a normal, functional life,” Dr. Tam says. “Physiatrists are trained in gait analysis and we work closely with prosthetists to ensure that patients are getting the proper prosthetic parts, best suited for them. We help bridge many gaps pre- and post-operation.”
Consistency and patience
When it comes to treatment plans, Dr. Tam says consistency and commitment are much more important than a fancy gym with special equipment.
“Recovery doesn’t happen overnight, and most patients only visit a physical therapist once or twice a week. Restoring function requires a lot of effort, and most of that comes from the patient committing to their exercises at home.”
At work, Dr. Tam coordinates her patients’ care and makes sense of their intricate, complicated needs. In her down time, she loves to use that patience and perspective to tackle 5000-piece jigsaw puzzles.
“I feel so much satisfaction when I find the right puzzle piece! Put on a crime podcast, and I’m good to go on a puzzle for hours,” she laughs.
Find Dr. Tam at PacMed clinics in Beacon Hill, Federal Way, and Renton. To make an appointment, call 1.888.472.2633 or click here.
For this primary care physician, food is foundational
From infant nutrition to chronic disease management, Dr. Kaba helps patients find custom solutions.
Christina Kaba, MD, has two children, aged 10 months and three years, and she had both of them while in the UCLA Internal Medicine residency program.
“I had no idea how I was going to breastfeed or pump at work: Was it going to be impossible? Was it something that was important to me?” she says. “The conversation around breastmilk versus formula is really charged! Parents end up feeling stigmatized either way.”
Lactation medicine is usually left to doctors who practice Pediatrics, Family Medicine and Obstetrics & Gynecology, but Dr. Kaba’s personal experience as a working mother helped her see how Internal Medicine physicians could also contribute to this care.
“There wasn’t a lot of focus on the lactating partner’s health in that first year raising a newborn. There’s so much you have to cover around the baby — some of that is around feeding, but there’s not much time for other concerns.”
Dr. Kaba is now board certified and practicing at Pacific Medical Centers (PacMed) Northgate, where she’s excited to collaborate with colleagues in Family Medicine, Pediatrics and Obstetrics to help cover all aspects of patients’ lives. That could mean scheduling appointments for parent and child back-to-back, or arranging a virtual visit when the newborn is (hopefully) napping.
Keys to a healthy lifestyle at any age
“Fed is first,” a mantra in newborn nutrition, aims to reduce stigma around breastmilk and formula, by emphasizing that feeding the baby is most important. Dr. Kaba applies a similar approach to nutrition and fitness in her adult patients.
“The best exercise is whatever you think you can do regularly,” she says. “And if we can change your daily diet to something sustainable for you, that’s the foundation for so much of our health.”
Dr. Kaba became more interested in the specifics of clinical nutrition during her UCLA residency, studying data and goal-setting strategies to care for common diseases like hypertension, cholesterol and diabetes through lifestyle changes.
“The path to a healthy lifestyle is different for everyone. I ask my patients about their background, their work and living situation, their income level and medical conditions. There’s a lot of stigma around weight, and that can be really demoralizing,” she says. “Pharmaceutical treatments are also part of the conversation, whether that’s to treat the disease or to help with weight loss.”
With chronic diseases, it can take time to find all the contributing factors to chronic diseases. Sometimes these concerns are addressed in an annual physical exam, but Dr. Kaba is also happy to schedule extra appointments with her patients to go into more depth.
“Since starting my practice on October 1 I’ve already had patients come in for a first visit, and then schedule a follow-up to talk about nutrition once we discover it’s a shared priority for both of us.”
To make an appointment with Dr. Christina Kaba at PacMed Northgate, 10416 5th Avenue NE, Seattle, WA, call 206-517-6700 or click here.
Bringing the easy warmth of a small-town doctor to patients catching up on primary care
After 35 years at his own private practice, Dr. McLaughlin is continuing care at PacMed Federal Way.
When Robert McLaughlin, MD moved to Federal Way in 1986, he brought a little bit of rural Illinois with him.
“I grew up in a small Midwestern town with one family doctor,” he explains, “And when I established a private practice in Federal Way I had a similar philosophy: care for everyone in the community, for whatever concerns they may have.”
After 35 years operating a walk-in clinic for local families, Dr. McLaughlin has moved his practice to Pacific Medical Centers Federal Way. His patients say they still feel like they’re getting that small-town service.
“Even if it’s a big fancy building, they still get to see good old Dr. McLaughlin,” he says. “PacMed has been great. I still feel like I’m working for myself, not a big conglomeration, and patients continue to be our top priority.”
35 years in Federal Way
Dr. McLaughlin still sees patients he’s known for three decades, as well as their children, grandchildren — and new patients too.
“I have one patient who tells me the same thing every time she sees me. She says, ‘thank you for saving my life.’” 20 years ago Dr. McLaughlin told her she was going to die unless she quit smoking, and she says she quit smoking that very day.
“Sometimes my words do carry weight,” he says. “It’s never as simple as telling a patient to quit smoking. You have to figure out what motivates each individual patient.”
The art of medicine… and classic cars
Motivating unique patients and tinkering with cantankerous classic cars are two interests that Dr. McLaughlin has held since his youth. The two passions are more similar than you might think.
“You have to bring an artistic quality to restoring classic cars, and there is an art to medicine, too,” he says. “You can tell the difference between a car that’s been thrown together and one that’s been assembled with care and attention.”
Dr. McLaughlin is clearly interested in the mechanics of fixing things—whether that’s refurbishing a paint job and gently coaxing an engine back to life, or treating a patient’s rash and mending broken bones. He puts time and care into each visit with his patients, talking with them to learn their concerns and then thoughtfully diagnosing both the issue and treatments.
It’s time to catch up on care
With the pandemic, many people put their health care on the back burner. But Dr. McLaughlin encourages everyone to visit their primary care provider. A wellness exam can uncover new issues and keep tabs on chronic conditions.
“Don’t put off those minor complaints. If it’s been there for a while and you’re wondering if it’s worth going to the doctor, the answer is yes.”
3 things to prioritize:
- Routine cancer screenings including colonoscopies and mammograms.
- Elective surgeries for joint replacements or minor cosmetic surgery.
- New or changing skin conditions which may indicate melanoma.
To make an in-person or virtual appointment with Dr. Robert McLaughlin at Pacific Medical Centers Federal Way, 31833 Gateway Center Blvd S, call (888) 472.2633 or visit click here.
Stomach problems: their cause, treatment, and prevention
In the November 2021 edition of Men’s Health Monthly, Neil Scott and Dr. Tom Walsh welcome PacMed’s Dr. Liz Broussard – one of the top Gastrointestinal physicians in the Pacific Northwest – to discuss stomach problems, their cause, treatment and prevention.
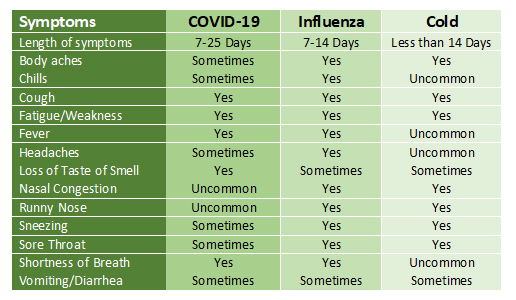
Flu, Cold, and COVID-19: How to tell the difference
When symptoms of seasonal illness set in, it won’t always be clear which infection you’re dealing with. Because it will be difficult to tell them apart, contact your provider to determine what care you may need, including testing.
- COVID-19 is a highly contagious respiratory illness. COVID-19 can have varying degrees of symptoms, from none to severe. Symptoms may include fever or chills, severe cough, sore throat and the loss of taste or smell. COVID-19 can cause medical complications, especially in higher-risk groups, and can result in hospitalization and death. If you think you’ve been exposed to COVID-19 or are experiencing symptoms, learn more about options for screening and receiving care.
- The flu is a contagious respiratory illness that can cause mild to severe illness, with symptoms such as fever, cough and body aches. Most people with the flu don’t need medical care or medication. However, the flu can be very serious and require medical attention. Contact your doctor if your symptoms worsen, are prolonged, or if you’re at high risk of flu-related complications. Testing may be necessary to confirm a diagnosis.
- With a cold, you may feel pretty crummy, but the symptoms (e.g., cough, sore throat, fatigue, etc.) are mild in comparison to viruses like the flu and COVID-19. Rest and many over-the-counter medications can help relieve symptoms.
Still unsure? Check your symptoms against this chart.
With the cold, flu and COVID-19 circulating in our communities, it’s more important than ever to stay healthy. The flu shot and COVID-19 vaccine is your best defense against serious illness and reduces the risk of spreading contagious diseases to friends, family and your community. And, it’s safe to get both the flu and COVID vaccine at the same time. Learn more about COVID-19 and flu shots.
Flu Season Questions Answered with PacMed’s Dr. Stewart
It’s flu season again—and lest we forget—the pandemic isn’t over yet, so it’s great timing to refresh our memories about flu season and getting our flu shots. I spoke with Family Medicine physician, Dr. Jimmie Stewart from Pacific Medical Centers (PacMed) about this topic this week.
Seattleite: When should we get the flu shot? And who do you recommend gets one?
Dr. Jimmie Stewart: I’d recommend people get it as soon as possible. Whenever you possibly can. I recommend anyone 6 months and up get vaccinated unless specifically recommended not to by their doctor.
Seattleite: Who’s at increased risk for getting the flu?
Dr. Jimmie Stewart: Anyone over 65 and those with lung disease (which can include smoking or asthma), heart disease, or who is immunocompromised are all at greater risk.
Seattleite: What would you say to people who say they don’t get the flu shot because it only reduces flu illness by an average of 40-60%?
Dr. Jimmie Stewart: No vaccine is perfect, but across the board, those who get the flu shot tend to have better outcomes if they are exposed to or get sick from the flu. It also helps decrease risk of hospitalization and can resolve a lot quicker.
Seattleite: Some people say they avoid getting the flu shot because they get super sick from it. What would you say to them?
Dr. Jimmie Stewart: Usually some symptoms is the appropriate response, which can last from 24 hours to a few days. That means your immune system is activating. Symptoms can range, but can include: lower energy, feeling unwell, nausea, and upset stomach. However, compared to getting the flu these side effects are mild, as flu symptoms can last weeks.
Seattleite: Do you have any advice on how to differentiate between COVID-19 and flu symptoms?
Dr. Jimmie Stewart: They are both viruses so they can be hard to differentiate, especially in the beginning phases. Both could have symptoms of fever, lower energy, shortness of breath, and a cough. The biggest telltale COVID-19 symptom might by losing your taste and smell. The best way to find out for sure is to get tested.
Seattleite: What do you think about getting the COVID-19 booster shot and the flu shot at the same time? Are there increased symptoms?
Dr. Jimmie Stewart: Yes, the flu shot can be co-administered with COVID-19 vaccines. The efficacy doesn’t change if you get the shots together or not. It’s hard to say for sure if it would cause more symptoms because it’s so variable. Some people still won’t experience any symptoms and some people feel unwell for a day or two.
Seattleite: As a doctor, what are you comfortable doing in your personal life, in terms of navigating Covid-19 risk?
Dr. Jimmie Stewart: I am playing it much safer because I do see immunocompromised patients and people at risk. I try to take precautions and avoid unnecessary exposure when possible. I think it is important to assess your own responsibilities and risk to determine what is safest for you, your loved ones, and your community. It’s important to be honest if you’re experiencing any symptoms and to take the appropriate steps to isolate and test.
Dr. Stewart is a family medicine physician at PacMed.
Salmon Croquettes with Dill Sauce

Feta-Sweet Potato Salad