Health Care in the Age of Coronavirus
 There have been mixed political messages on how COVID-19 is spread but this much is not in dispute by health experts— it is very contagious, and people are advised to limit exposure wherever and whenever possible. No wonder, then, that telehealth is an increasingly popular way to access medical care, especially for the most vulnerable populations.
There have been mixed political messages on how COVID-19 is spread but this much is not in dispute by health experts— it is very contagious, and people are advised to limit exposure wherever and whenever possible. No wonder, then, that telehealth is an increasingly popular way to access medical care, especially for the most vulnerable populations.
While non-experts use the words telehealth and telemedicine interchangeably, they are not the same. According to the American Academy of Family Physicians, “telemedicine is the practice of using technology to deliver care at a distance. A physician in one location … to deliver care to a patient at a distant site. Telehealth refers broadly to electronic and telecommunications technologies and services used to provide care and service at a distance.” It’s important to note that during the coronavirus pandemic, the Centers for Medicare & Medicaid Services lifted some limitations on telehealth reimbursements.
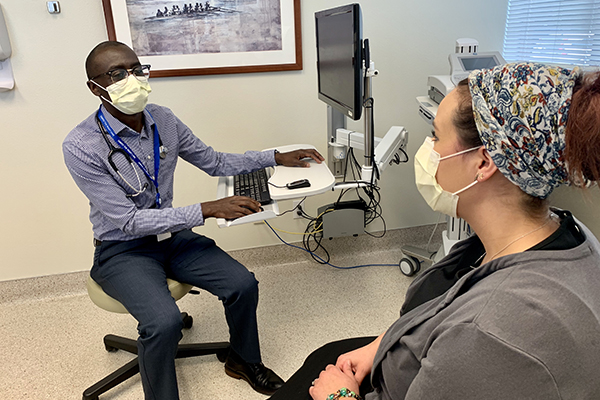
Simon Katumu, a primary care provider with Pacific Medical Centers (PacMed), notes a definite rise in this model of care. “During the pandemic, we’ve used telehealth much more, utilizing tools such as telephone consultations, Zoom meetings, and PacMed’s MyChart.” The latter offers online access to a variety of services including test results, prescription renewals, and virtual appointments with a health-care provider.
The benefits of using these tools are clear. “They help reduce exposure in the pandemic and are also convenient,” says Katumu. “We’ve seen great benefits for our patients.”
He says that initially, the thought was that older patients may not warm up to this technology but that hasn’t been the case. “They can do it or get assistance from someone who’s tech-savvy. It hasn’t been much of a problem.”
Katumu acknowledges there are limitations to tech. “We can’t draw blood virtually. We can’t complete physical examinations, like listen to hearts and lungs. So, it’s not a replacement for face-to-face care but it is a great addition to our toolkit.”
Security is also an issue when sharing sensitive medical information remotely. PacMed is partnering with Providence to use a dedicated, secure portal for patient visits through Zoom. The enhanced measures include encryption, meeting identifications, and verification to ensure that the patient’s telehealth visit is a private and secure experience. Even so, patients are advised to have secure systems at home and to find out what security measures are in place with their particular health care providers.
Another model of care that reduces trips to the doctor is mobile urgent care. “We like to say we’re bringing back the house call,” says Valerie Rose, community engagement manager with DispatchHealth, a new company in Washington state that provides advanced medical care for urgent and non-emergency medical needs. “We do an initial risk-assessment by phone,” she explains. “Within 90 minutes a care team arrives, which includes a physician’s assistant or nurse practitioner along with a medical technician.”
DispatchHealth offers a variety of services to all ages, from flu shots to stitches, and is especially appealing to older folks, Rose says. “There is no travel, no exposure, and most services are covered by insurance, Medicare, and Medicaid.”
Plus, there’s the luxury of time. “When was the last time you had 45 minutes of undivided attention with a medical provider?”
In addition, doctor referrals are not needed and it’s not as expensive as a trip to the emergency room. “We are a great adjunct to primary care,” says Rose. DispatchHealth is currently testing and exploring telehealth options in select markets to expand their house call model.
As devastating as COVID-19 is, it has driven innovative ways in which people access medical care. And the genie is unlikely going back in the bottle.
“I do think it’s here to stay,” says PacMed’s Katumu. “I think we’ll maintain what we have at this point and I expect it will grow and expand in the future.”